Benchmarks
View scores and output across OCR models spanning many document categories.
Want to run these evals on your own documents?
Talk to Sales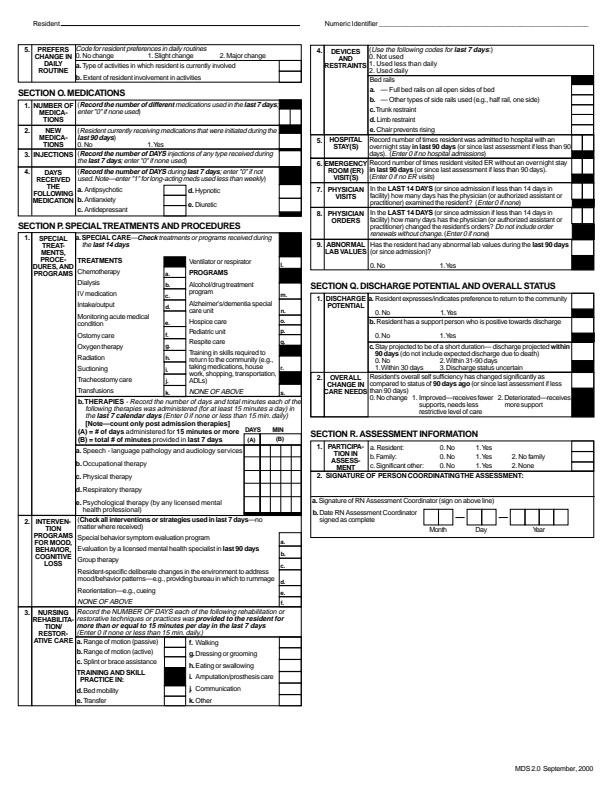
Resident
Numeric Identifier
| 5. PREFERS CHANGE IN DAILY ROUTINE |
Code for resident preferences in daily routines
0. No change 1. Slight change 2. Major change |
| a. Type of activities in which resident is currently involved | |
| b. Extent of resident involvement in activities |
SECTION O. MEDICATIONS
| 1. NUMBER OF MEDICATIONS | (Record the number of different medications used in the last 7 days; enter "0" if none used) |
| 2. NEW MEDICATIONS |
(Resident currently receiving medications that were initiated during the last 90 days)
0. No 1. Yes |
| 3. INJECTIONS | (Record the number of DAYS injections of any type received during the last 7 days; enter "0" if none used) |
| 4. DAYS RECEIVED THE FOLLOWING MEDICATION |
(Record the number of DAYS during last 7 days; enter "0" if not used. Note—enter "1" for long-acting meds used less than weekly)
a. Antipsychotic b. Antianxiety c. Antidepressant d. Hypnotic e. Diuretic |
SECTION P. SPECIAL TREATMENTS AND PROCEDURES
| 1. SPECIAL TREATMENTS, PROCEDURES, AND PROGRAMS |
a. SPECIAL CARE—Check treatments or programs received during the last 14 days
b. THERAPIES—Record the number of days and total minutes each of the following therapies was administered (for at least 15 minutes a day) in the last 7 calendar days (Enter 0 if none or less than 15 min. daily) (Note—count only post admission therapies)
a. Speech—language pathology and audiology services b. Occupational therapy c. Physical therapy d. Respiratory therapy e. Psychological therapy (by any licensed mental health professional) |
|||||||||||||||||||||||||||||||||
| 2. INTERVENTION PROGRAMS FOR MOOD, BEHAVIOR, COGNITIVE LOSS | (Check all interventions or strategies used in last 7 days—no matter where received) | |||||||||||||||||||||||||||||||||
| Special behavior symptom evaluation program | ||||||||||||||||||||||||||||||||||
| Evaluation by a licensed mental health specialist in last 90 days | ||||||||||||||||||||||||||||||||||
| Group therapy | ||||||||||||||||||||||||||||||||||
| Resident-specific deliberate changes in the environment to address mood/behavior patterns—e.g., providing bureau in which to rummage | ||||||||||||||||||||||||||||||||||
| Reorientation—e.g., cueing | ||||||||||||||||||||||||||||||||||
| NONE OF ABOVE | ||||||||||||||||||||||||||||||||||
| 3. NURSING REHABILITATION/ RESTORATIVE CARE | Record the NUMBER OF DAYS each of the following rehabilitation or restorative techniques or practices was provided to the resident for more than or equal to 15 minutes per day in the last 7 days (Enter 0 if none or less than 15 min. daily) | |||||||||||||||||||||||||||||||||
| a. Range of motion (passive) | ||||||||||||||||||||||||||||||||||
| b. Range of motion (active) | ||||||||||||||||||||||||||||||||||
| c. Splint or brace assistance | ||||||||||||||||||||||||||||||||||
| TRAINING AND SKILL PRACTICE IN: | ||||||||||||||||||||||||||||||||||
| d. Bed mobility | ||||||||||||||||||||||||||||||||||
| e. Transfer | ||||||||||||||||||||||||||||||||||
| f. Walking | ||||||||||||||||||||||||||||||||||
| g. Dressing or grooming | ||||||||||||||||||||||||||||||||||
| h. Eating or swallowing | ||||||||||||||||||||||||||||||||||
| i. Amputation/prosthesis care | ||||||||||||||||||||||||||||||||||
| j. Communication | ||||||||||||||||||||||||||||||||||
| k. Other |
| 4. DEVICES AND RESTRAINTS |
(Use the following codes for last 7 days)
0. Not used 1. Used less than daily 2. Used daily |
| a. — Full bed rails on all open sides of bed | |
| b. — Other types of side rails used (e.g., half rail, one side) | |
| c. Trunk restraint | |
| d. Limb restraint | |
| e. Chair prevents rising | |
| 5. HOSPITAL STAY(S) | Record number of times resident was admitted to hospital with an overnight stay in last 90 days (or since last assessment if less than 90 days). (Enter 0 if no hospital admissions) |
| 6. EMERGENCY ROOM (ER) VISIT(S) | Record number of times resident visited ER without an overnight stay in last 90 days (or since last assessment if less than 90 days). (Enter 0 if no ER visits) |
| 7. PHYSICIAN VISITS | In the LAST 14 DAYS (or since admission if less than 14 days in facility) how many days has the physician (or authorized assistant or practitioner) examined the resident? (Enter 0 if none) |
| 8. PHYSICIAN ORDERS | In the LAST 14 DAYS (or since admission if less than 14 days in facility) how many days has the physician (or authorized assistant or practitioner) changed the resident's orders? Do not include order renewals without change. (Enter 0 if none) |
| 9. ABNORMAL LAB VALUES |
Has the resident had any abnormal lab values during the last 90 days (or since admission)?
0. No 1. Yes |
SECTION Q. DISCHARGE POTENTIAL AND OVERALL STATUS
| 1. DISCHARGE POTENTIAL |
a. Resident expresses/indicates preference to return to the community
0. No 1. Yes |
|
b. Resident has a support person who is positive towards discharge
0. No 1. Yes |
|
|
c. Stay projected to be of a short duration—discharge projected within 90 days (do not include expected discharge due to death)
0. No 1. Within 30 days 2. Within 31-90 days 3. Discharge status uncertain |
|
| 2. OVERALL CHANGE IN CARE NEEDS |
Resident's overall self sufficiency has changed significantly as compared to status of 90 days ago (or since last assessment if less than 90 days)
0. No change 1. Improved—receives fewer supports, needs less restrictive level of care 2. Deteriorated—receives more support |
SECTION R. ASSESSMENT INFORMATION
| 1. PARTICIPATION IN ASSESSMENT |
a. Resident:
0. No 1. Yes |
|||
|
b. Family:
0. No 1. Yes |
2. No family | |||
|
c. Significant other:
0. No 1. Yes |
2. None | |||
| 2. SIGNATURE OF PERSON COORDINATING THE ASSESSMENT: | ||||
| a. Signature of RN Assessment Coordinator (sign on above line) | ||||
| b. Date RN Assessment Coordinator signed as complete |
|
MDS 2.0 September, 2000